Our vision of a national health platform foresees a trustworthy information architecture within the healthcare sector that aims to streamline the management of health-related information and render top-tier information and data more readily available. This contribution offers a bird’s eye view of the digital ecosystem we’ve envisioned and outlines the key stakeholders, roles and processes involved.
The core service provided by this ecosystem is a customized compilation of quality-assured information and services that are tailored to individual information needs over time (see Discover more, search less). This service helps ensure that patients receive information that is pertinent to their needs when they need it. By consolidating a variety of content from accredited providers, the platform curates trustworthy information and services. Tailored to users’ individual contextual factors, the curated information and services are further refined to cater to specific situational support requirements (see Without context, everything is nothing).
This process-driven guidance, coupled with tailored-to-the user information and service offerings, not only fosters well-informed decision-making but also advances health literacy, thereby making a substantial contribution to personal health management (see Health literacy and infodemics). However, making this product vision a reality requires more than simply providing a technical platform equipped with algorithmic systems. Above all, it requires the constructive, collaborative engagement of the full array of relevant actors and players. Collectively, they constitute the digital ecosystem in which the national health platform operates. They target shared objectives and benefit from the rewards of their collective engagement (refer to Benefit model for a national health platform).
Brokering trustworthy health information and services
A key element of the platform centers on the curation of information and service providers, as well as the brokering of trustworthy health-related information and service offerings. The platform is not designed for the creation of original content. The platform does not engage in generating original content; rather, it excels at cultivating an ecosystem wherein the platform’s initiator and operator do not shoulder the sole responsibility for developing all functions and services. Instead, their focus lies in establishing the framework that empowers partners to seamlessly integrate their services and applications into this ecosystem. Thus, the platform does not autonomously produce content and offerings; rather, it functions as a broker for context-specific health information and services.
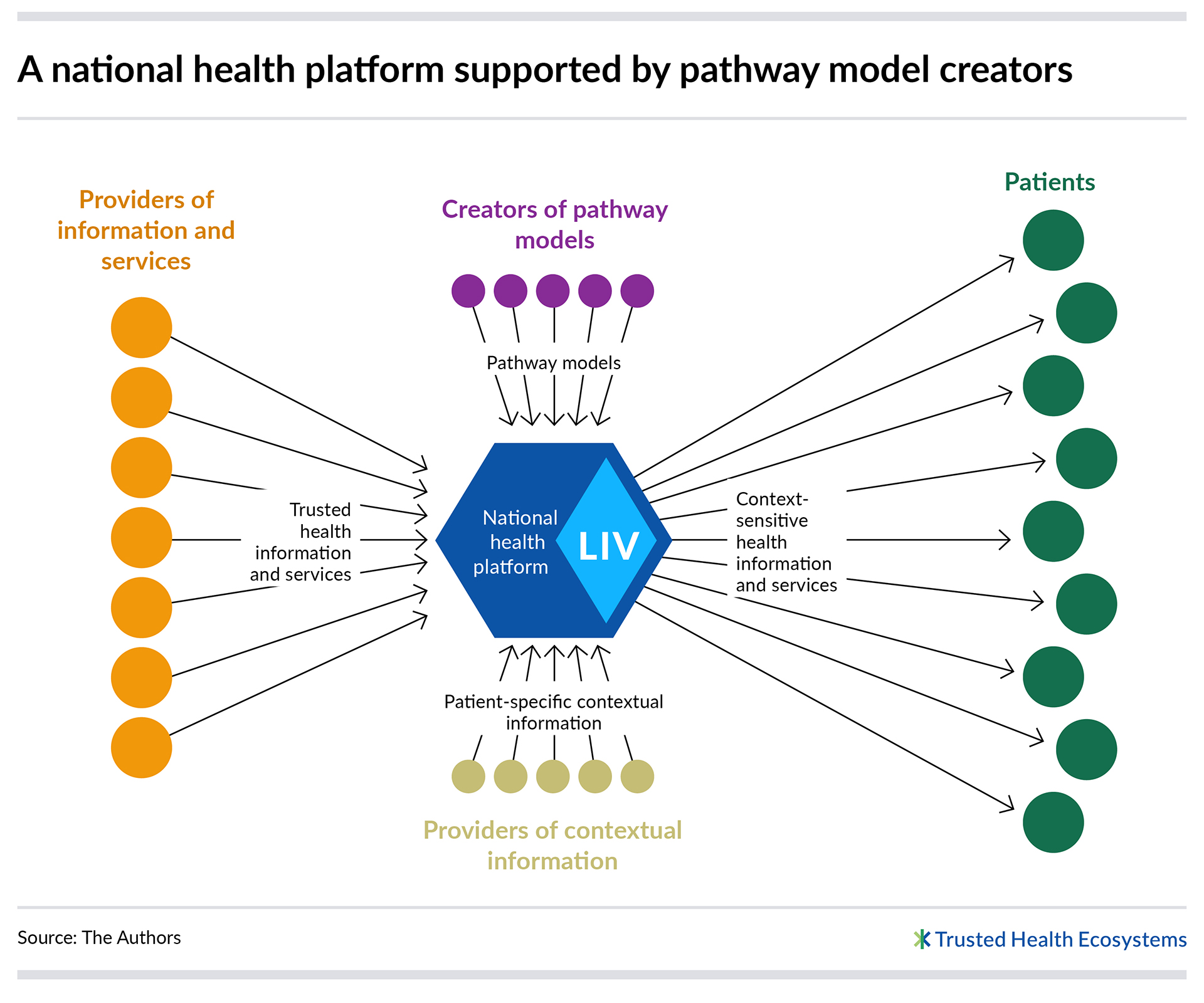
This “brokering principle” revolves around the role of an intermediary that bridges supply and demand. The “broker” provides the infrastructure and delivers a user-friendly interface, thus facilitating interaction between the two sides. Such platforms often include rating systems, offer recommendations, or contribute to personalized offerings. We’ve applied this approach in our blueprint for a national health platform. The platform thus acts as a broker, connecting providers of health information and digital services on one end with patients on the other. By tailoring the presentation of available options to align with a patient’s specific requirements, the platform enhances its brokering service.
As a central figure within the digital ecosystem, the platform operator shoulders a range of responsibilities to ensure the seamless operation of the platform. This encompasses the provision of essential technological infrastructure, including software, servers, databases, networks, interfaces, and an array of technical resources. The tasks of a platform operator further encompass delineating platform regulations, fostering connections among participating entities, promoting interactive engagement, establishing a trustworthy space of interactions, and ultimately, expanding and scaling both the platform and the encompassing ecosystem.
Given this diversity of tasks and the anticipated scope of the digital ecosystem, the platform operator faces substantial demands. It is imperative that the governing body maintains independence and secures the acceptance of all participating entities. Moreover, it’s crucial to recognize that governmental institutions have limitations, as information activities administered by the state are bound by specific legal prerequisites (see ). Thus, to ensure legal clarity, it is advisable to establish a platform that is rooted in civil society and which is not administered by the state.
In the case of the national health platform, it seems advisable to delegate specific tasks within the ecosystem to distinct entities or bodies, conceptualizing the ecosystem as an overarching organization. Effectively managing the governance and operations of this digital ecosystem could involve distributing responsibilities across various organizational units to accommodate the complexity and diversity of roles, functions and tasks. All participating organizations could then be brought together under a non-profit and independently funded holding structure (see Ownership: Public or private?).
To consolidate a diverse array of offerings on the platform and harness the innovative capabilities of various stakeholders, the ecosystem should remain open to state-run, civil society and commercial information and service providers, whose role involves contributing their offerings and thus breathing life into the platform. Relevant offerings include not only conventional information portals but also digital services, such as those that allow patients to schedule doctor appointments or locate specialists.
A prerequisite for participation in the ecosystem is meeting clearly defined quality requirements that must be demonstrated at the provider level. Our concept thus envisions a certification procedure that focuses on both structural and process quality (see InfoCure: Making quality visible). All providers with a valid certificate can add their information and services to the ecosystem. The result is a trustworthy pool of information and services that have been sourced exclusively from verified providers.
Searching for trustworthy health information is often no less difficult than looking for a needle in a haystack. The challenge for patients lies in filtering out the information that is truly relevant to their specific situation. The national health platform can provide assistance in this regard by providing personalized information with exceptional precision that is embedded within a structured learning and interaction framework known as a Patient Information Pathway (see ).
Within these information pathways, platform users receive customized information and service offerings that are tailored to their specific phase of illness, coping and care. These pathways follow condition-specific patterns or pathway models. While basic condition-related information is provided with the initial diagnosis, subsequent stages frequently entail assessing specific treatment options. Particularly in the case of chronic conditions, managing the illness often becomes the focal point of attention.
By following such patterns, the anticipated trajectories of information needs can be modelled for a variety of conditions. These models can be used to automatically structure information in chronological order, which allows patients access to information they might not have actively sought. This could include pointing them toward legal and social matters relevant to their specific treatment phase.
In addition to providers, the ecosystem also needs pathway model creators to design pathway models. This role requires having the expertise to define templates for information and support needs and could be taken up by various decentralized actors, such as professional societies or patient advocacy groups. These actors can help create a large number of pathway models in a very short period of time.
While templates structure information, they do not account for where patients stand along their timelines, potential supplementary information needs, or decisions to be made during a course of treatment. Information needs can vary substantially and depend on factors like whether a patient has opted for surgery or a more conservative treatment.
In order to provide a truly tailored-to-needs set of offerings and create customized information pathways, pathway models must be adaptable to changing contexts. This could involve using periodic self-reported input from users. However, extensive data collection of such inputs is inconvenient for users, often impractical, and raises the spectre of the search engine problematic. But how can the platform “know” what information its users need in a given moment?
The key to delivering a personalized offering lies in factoring in a wide spectrum of contextual information that can be easily and automatically obtained with the individuals’ consent (see ). Providers of contextual information thus form the third relevant group of actors within the digital ecosystem.
Potential sources of pertinent contextual information include electronic health records, which, within an advanced Telematics Infrastructure 2.0, could provide vital insights into the situational information needs of patients. Similarly, the management systems used by hospitals and physicians’ offices, as well as digital health applications or fitness trackers, could serve as sources in this regard.
Contextual information is already present in digital systems and would no longer need to be captured through a separate process. Leveraging these resources within the digital ecosystem to personalize health information and services creates a clear benefit for patients by mitigating information overload while improving the quality of information provided. Contextual information can also be used to proactively inform patients, remind them of tasks, or tailor how information is presented to align with individual preferences.
High-quality collaboration
A truly user-centered offering can only come to fruition through the collaborative interaction of different types of participants. Providers of information and services, creators of pathway models, and providers of contextual information each bring a crucial element to the functionality of the ecosystem. Just like the pieces of a puzzle, their contributions fit together, creating added value as a whole.
In order to instill user trust, the platform must adhere to stringent quality standards. However, given the platform’s openness to a vast number of participating entities, meeting these standards is far from straightforward. A key aspect of quality management is rooted in the aforementioned certification of information and service providers. Yet, this alone falls short, as ensuring quality must extend across all processes within the ecosystem. Pathway model creators and contextual information providers must also meet clear quality or qualification standards that align with their respective roles.
LIV – An easy to use, personalized and trustworthy user interface
The synergies created by the variety of actors participating in the national health platform are expected to create significant and tangible added value for patients. Regarding products, there are likely numerous pathways through which these synergies can materialize. To facilitate a shared understanding of what our product vision entails, we have articulated in detail one such pathway and developed a prototypical design that showcases what the national health platform might look like from the patient viewpoint (see Discover more, search less – prototype of a national health platform).
Our concept envisions a platform with a user interface that is tailored specifically to the patient’s needs and is available as an app as well as a website. We’ve named the interface “LIV,” which stands for the German concepts of “leicht” (easy), “individuell” (individual), and “vertrauenswürdig” (trustworthy). LIV is designed to provide optimal support to patients, both proactively and during targeted searches. It’s primary design principle is to mitigate information overload while offering only high-quality information and services. The content provided through LIV is thus highly personalized, and the timing of its delivery is driven by contextual information.
If implemented, LIV would be available to millions of people and thus the national health platform’s most visible component. However, the platform would require additional components in order to facilitate seamless interaction among the various groups of actors. For example, the platform would need more user interfaces for ecosystem participants that would allow them to register new health information and services or to create templates for patient information pathways. Integration interfaces would also be needed to connect other IT systems, such as those used by context providers (cf. Initial thoughts on the technical structure of the national health platform).
Find, understand, appraise and apply
The twin goals of our product concept for the national health platform are to streamline health information management and promote health literacy. Health literacy involves having the skills to find, understand, evaluate and apply health-related information. Research suggests that digital information overload poses a challenge to nearly half of the European population. The core service of the national heath platform we’ve conceived addresses this concern and operates across all four levels of health literacy.
Find: Users no longer have to actively seek out pertinent information. Instead, relevant content and services are proactively presented to them. This shift from a “push” to a “pull” communication model offering personalized information streamlines search efforts, preventing users from becoming lost in the sea of information.
Understand: The ecosystem defines minimum standards for content clarity and digital application usability. In addition, the complexity of texts can be determined automatically. Users can then select information that is suited to their (self-reported) level of health literacy.
Appraise: A cornerstone of the ecosystem is the quality-centric selection of providers of information and digital services. As part of the proposed national-level certification process, providers would be audited at regular intervals. This helps create a trusted space for patients in which the risk of misinformation and data misuse is mitigated.
Apply: Information gains practical relevance when it leads to actionable decisions. The personalized compilation of information and digital services makes it easier for users to modify their behavior, make informed choices, and translate knowledge into practice.
Additional benefits of the national health platform
In addition to its core service, the concept of a national health platform harbors several opportunities to create additional benefits and engage more actors in the digital ecosystem:
- Distribution partners: The quality-assured health information and services available on the national health platform could be distributed through alternative channels. These distribution partners might encompass other platforms that specialize in delivering health-related content and services. Other candidates include digital health applications that require curated information and directly integrate it into their solutions.
- White-label solutions: In principle, LIV could potentially be provided as a white-label patient interface. Interested partners could incorporate this application into their own offerings and infuse it with their branding. Such a move would further amplify the reach of LIV.
- Anonymized data for research: The national health platform processes data that not only benefits patients directly but could generate additional value. By means of aggregated analysis, the provision of fully anonymized data or creation of synthetic data sets, the platform could make a valuable contribution to health services research.
- Internationalization: Although conceived for a national setting, the envisaged health platform has the potential for international scalability. Despite differences in healthcare systems, the platform’s principles, roles, and even software could be adapted to suit other national contexts. Over time, an international network of nationally anchored platforms might materialize in which each network adheres to shared standards, exchanges insights and data, and thereby contributes to establishing a global infrastructure of trust.